Chronic Prostatitis and Chronic Pelvic Pain Syndrome (CPPS)
Chronic Prostatitis or Chronic Pelvic Pain Syndrome (CPPS) are often considered synonymous where the pain in the pelvis is of a persistent nature. In Prostatitis, there may be an infection affecting the prostate gland and about 5-10% are actually bacteria related while the vast majority are related to inflammation or non-specific pain syndromes. Prostatitis can affect men at any age and accounts for about ¼ of all pelvic pain, genital or urinary conditions in young to middle-aged men. Where pain persists after a period of time and after the medicine has failed to resolve pain, CPPS or Chronic Prostatitis is a diagnosis often assigned. Prostate Milking can help in some circumstances ........... many men find a rectal examination which includes massage and drainage of the swollen prostate gland helpful in decreasing their pain
Acute Prostatitis
The least common form of the condition manifests with an increased frequency of micturition, particularly at night. There is often pain in the pelvis and genitals, and there are other signs of infection including vomiting, fever, and chills. This condition would make you feel quite ill and requires prompt treatment. Left untreated symptoms lead to a drop in blood pressure, confusion, and increased mortality. Prostate Milking can help in some circumstances ........... many men find a rectal examination which includes massage and drainage of the swollen prostate gland helpful in decreasing their pain
Chronic prostatitis
Diagnosed in situations where the symptoms of prostate infections are recurrent. The symptoms are much less severe than in acute states but they are often difficult to treat with many trials of antibiotics proving unsuccessful and the patient suffering recurrent pain and symptoms.
Chronic Pelvic Pain (CPP)
Pain is considered ‘chronic’ when it has been present for more than 3 months. Where pain persists but inflammation and bacteria are absent a condition of chronic non-bacterial prostatitis or chronic pelvic pain can be assigned. This condition is the most common form of pelvic pain and accounts for up to 90% of cases. You may have been seen by a colorectal specialist or urologist with multiple tests and only negative findings. CPP is therefore a diagnosis often determined by a process of elimination.
Signs and symptoms are varied, mixed, and often do not have a clear algorithm for diagnosis. Clinical examination with a solid patient history is essential. However, typical symptoms may include:
- Low back pain, abdominal, buttock, or groin pain
- Urinary symptoms
- Rectal symptoms
- Pain on sexual activity
- Loss of Libido, erection, or the ability to ejaculate
- With Low mood, anxiety, and often difficulty with relationships
Assessment
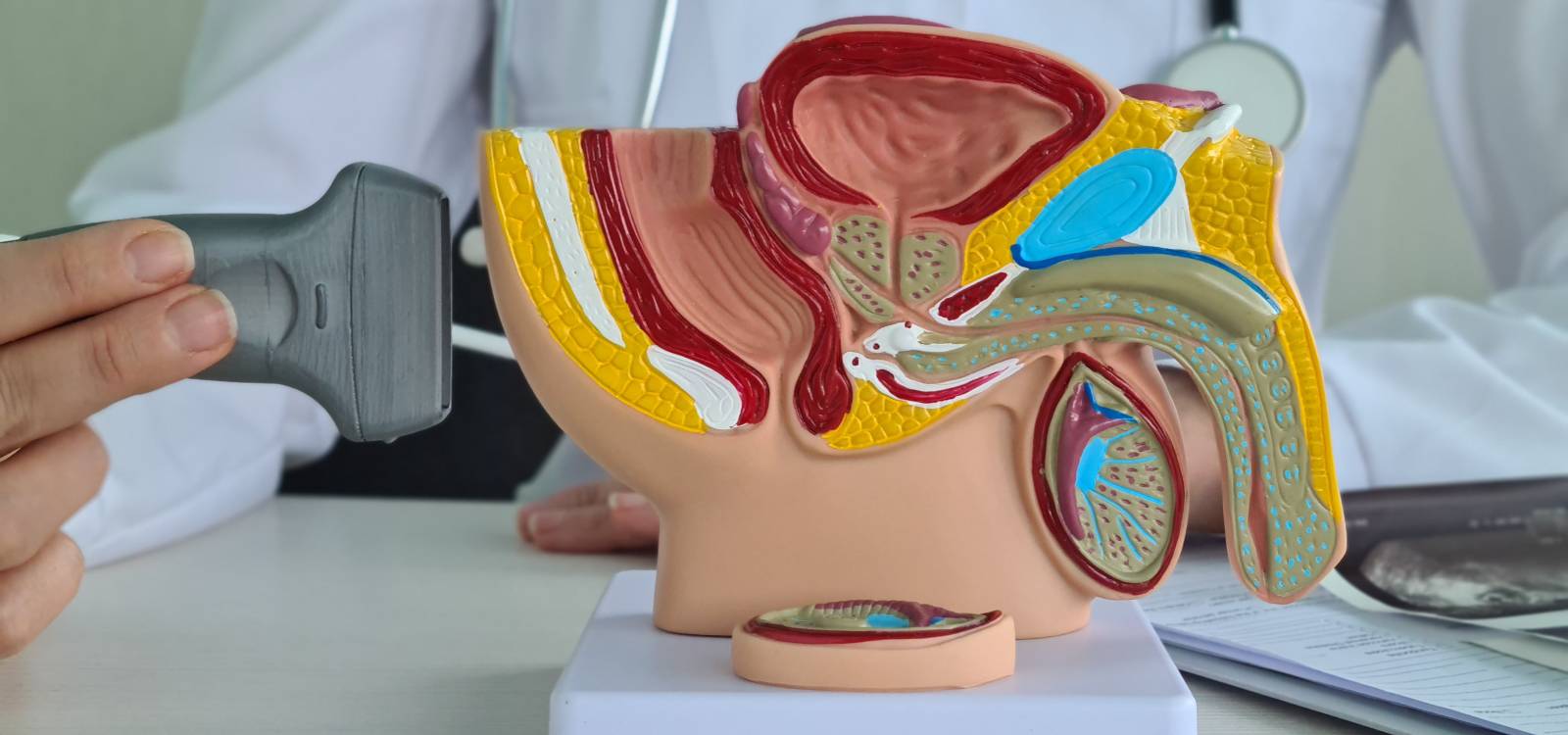
Our pelvic assessment program uses a subjective comprehensive examination where we will encourage dialogue from the patient to discuss their problem in as much detail as possible. We will use differential questioning to hone in on the possible causes of your problem. The history of any condition as told by the patient reveals much more (in many cases) than any test or examination. Therefore, this phase may take a little time to ensure we get all the important information down. Some questions may be of a sensitive nature. We will always explain why we need to ask such questions and will use our knowledge of pelvic anatomy and skeletal models/diagrams to help with our explanation.
The examination will include the lumbar spine, pelvis, hips, and pelvic muscles. Most of the examination will be external but may include direct palpation of the perineum or instruction to the patient to palpate their own perineum (saddle region between the anus and scrotum). We may also palpate on the inside of the pelvis. This is called an internal examination and allows the physiotherapist to determine the presence of trigger points inside the pelvis that may be inhibiting muscle function or causing pain. Gaining access requires palpation through the anus. This is by no means an absolute necessity but remains the gold standard for assessment of the pelvic floor. Total understanding and a complete explanation, and only after consent in a written format are any form of internal examinations conducted. Dynamic ultrasound may also be used to assess the pelvic floor function. For patients who are incontinent, this is often the only method of assessment.
Once we have completed both phases of the examination, we will then formulate an action plan with the patient and begin treatment.
If you are in any doubt as to whether we can help, please contact us to discuss and we will advise accordingly.
Other useful information can be found at Prostate Cancer UK We recommend the Squeezy App for pelvic floor exercises at home